Navigating POTS and EDS: Insights from Abby Gordon
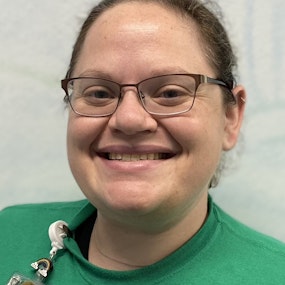
In this enlightening episode of The Modern Pain Podcast, we are honored to have Abby Gordon, an experienced professional in the world of physical therapy, delve into complex conditions like Postural Orthostatic Tachycardia Syndrome (POTS) and Ehler's Danlos Syndrome (EDS). Abby brings her unique expertise from both the sports therapy world and her significant experience in treating chronic conditions. This conversation aims to shed light on how PTs can navigate the challenging landscape of these disorders, balancing cutting-edge therapies with practical patient care.
Abby Gordon shares her personal journey from working on the sidelines of sports events to diving deep into the clinic to manage POTS and EDS. Her insights are not only invaluable for clinicians seeking a better understanding of these complex conditions, but also for patients aiming to make sense of their difficult journeys with chronic pain. With Abby's varied background in physical therapy, the discussion provides a multi-dimensional view on how to approach patient care with empathy, skill, and the latest evidence-based practices. Subscribe now and don't miss this in-depth look into the world of physical therapy and its role in managing POTS and EDS.
*********************************************************************
📸 - Follow us on Instagram - https://www.instagram.com/modernpaincare/
🐦 - Follow us on Twitter - https://www.twitter.com/modernpaincare/
🎙️ - Listen to our Podcast - https://www.modernpaincare.com
____________________________________
Modern Pain Care is a company dedicated to spreading evidence-based and person-centered information about pain, prevention, and overall fitness and wellness
Mark Kargela:
If you've been practicing for about 10 years or more, you're likely seeing some newer conditions at least conditions that weren't previously diagnosed entering your clinic doors. Ehlers-danlos Pots and Mass Activation Syndrome can occur together and are more commonly walking through clinic doors looking for your help. This week we have Abby Gordon, a physical therapist at Seattle Children's Hospital, in to share her expertise in helping people dealing with these conditions. We speak to common patterns, we see the role of lifestyle medicine, working with parents of kiddos with these disorders and more. This is a great conversation that I think you will get some significant value of as these conditions walk through your clinic door. Enjoy.
Speaker 2:
This is the Modern Pain Podcast with Mark Kargela.
Mark Kargela:
Welcome to the podcast, Abby.
Abby Gordon:
Thanks for having me, Mark.
Mark Kargela:
You know we've chatted a bit before and I've definitely followed you a bit online. This, what spurred this, our discussion today, is to clinicians who are kind of the front lines of trying to deal with some conditions that are, you know, still kind of new and we'll talk about those today, of course, but Abby has some great content. We'll link her Twitter follow. She's always got some good commentary and things on Twitter X, whatever the heck we're calling it these days. Abby, if you don't mind, I know about your background and things, but maybe the audience doesn't. If you don't mind introducing yourself a little bit and kind of your background, Sure.
Abby Gordon:
Hello everyone, abby Gordon, I'm a sports physical therapist at Seattle Children's Hospital. I'm about to have been there for seven years and I'm also about to hit 10 years as a physical therapist, so I feel like I'm hitting some nice landmarks in my career. I was the team physical therapist for the Seattle Storm WNBA basketball team for eight years, so I did a lot of work sports related, specific to women's sports, but in the clinic I started to gain a lot of interest around chronic pain, and so I'm part of the pain management clinic at Seattle Children's and I basically just treat kids between ages five and 21 for musculoskeletal injuries, sports related injuries or chronic pain. So it's kind of where.
Mark Kargela:
I'm at. That's a interesting. I like it because it's kind of the similar spread. I mean I see everything from the pediatric athlete to the geriatric chronic pain debilitated and everything in between. So it's fun to have that spread, as you think. I mean nothing wrong with niche and down and really folks, not one thing but I'm definitely similar where I like to see the gamut of things and then still obviously the chronic pain. That's obviously how our discussions has happened. We both like to nerd out and chat about chronic pain, so it's obviously a fun topic to talk about in our eyes. What we wanted to talk about today because I had reached out and Todd Davenport hopefully we're gonna get him on the podcast too Just to talk about some of the new conditions. I guess new conditions as far as being more recognized and more something that we're seeing come through our clinic door, one being Ehlers-Danlos disease. What's been your experience at Seattle Children's with that? I mean in your 10 years you're hit the decade mark right now what's been your experience with that diagnosis as far as the prevalence of it in your practice? Have you seen that kind of uptick that it seems to be? Folks are seen around the country world, for that matter.
Abby Gordon:
Yeah, I've seen a pretty good handful of teenagers who've had Ehlers-Danlos, almost all of them female but not all, which has been interesting because the females have not presented the same as the male did. But I've seen them for two kind of different clusters of things. So one cluster has been joint dislocations, where they ended up having surgery at several shoulder dislocations and a lot of the knee, where we see the MPFL surgery that I feel like. I feel like if you're an adult orthopedics you see so much about ACLs but when you do peeds you have the ACL group and the MPFL group, which is the medial patella femoral ligament, and when you dislocate your patella that's part of the retinacular structures and so they reconstruct that to keep your patella in place. So I see a lot of those in the rehab is kind of similar to ACLs. The protocols are a little different but I see that as one cluster for these kids where they've had a really big injury but they're playing sports, they're active and they don't really have a lot of other things going on. And then there's this other group which is usually coming from our chronic pain clinic where they have like systemic everything they have fatigue, they have dysautonomia, potentially pots they might have like. I usually share these patients with our occupational therapists because they often have a lot of hand related issues. There's assistive devices involved and, as the sports PT and the team, I don't usually do a lot of work with our assistive device ordering and with orthotics and prosthetics and so we kind of they end up being more of like a team approach patient who sees a lot more medical where there's medications on board probably cardiology is on board, neurology like it's. They're very different ends of the spectrum, considering they're the same diagnosis but, like you know, we have gymnasts who are super flexible, who have an injury and it comes to find out that they also have the diagnosis or you have kind of the opposite end of the spectrum.
Mark Kargela:
Yeah, it seems there's probably a lot of folks operating in the world with that diagnosis before it was even recognized as a diagnosis. Just they were loose, jointed, double jointed, all the things that we used to say. I have friends and you know, folks that you come across in the past who always could do those like party trick things with shoulders and things, and oftentimes the EDS folks are folks. Yeah, I can do all these different things. I think well, let's pump the brakes on exposing that too much. I'd love to. We're gonna come back to the first group because I definitely work with some of those folks as well where they're athletic, they're kind of actively engaged in sport and activity and you know, obviously, injuries and things where there's not as much of that passive support, where things can get strained, injured and so on. The group with the more systemic dysregulation. I'm curious what you've seen. I've seen definitely some of that. I'm working with somebody right now and I only saw for the first appointment and really just sat and talked and laid out a plan of what we would look to do and younger person who's really and sad to see it. Look, because I know you've seen some tough stories your way too where functioning kids which they should be enjoying school and doing all the things kids should be doing and they get these illnesses that flip their world upside down, not able to function, not able to get to school, not able to do the things that everybody in their age groups doing. I'm wondering what you've seen as far as and maybe what you do at CL Children's in your group, because I know it's obviously a team approach. Have you seen any adverse childhood events type things or trauma backgrounds with some of these folks? I know it's definitely been something. That has been not all, but a pretty sizable percentage of folks that I've seen who have this systemic dysregulation. When you start gaining a therapeutic alliance and discussing all the things that can influence systemic dysregulation we talked about trauma and things I'm curious what your view has been and what you've seen.
Abby Gordon:
Well, I think, first and foremost, like Ehlers-Danlos is not one thing, it's a list of different genetic possibilities. So we potentially need to recognize that there are diagnostic criteria it's almost always genetic studies but that the hypermobility type doesn't really have a specific genetic finding. So a lot of the times these kids come in and they're like their diagnosis is just hypermobility and all you have is a bait and score nine out of nine and then it's like take them in PT and help them, but what they really have is hypermobility with GI dysfunction, usually some sort of like allergies, like something immune related, where either like food allergies or medication allergies, or they have Crohn's or C lax and like those are such different things in and of themself. And so there's like those things which come with medications. And then we have some a lot of the time like a brain fog type descriptor of either like a lot of fatigue or just energy challenge, difficulty tolerating activity, even at like baseline, yeah, and then potentially even more than that. So, and also I would say I don't know the number from the literature, but I would bet that it's probably something like 20% around the autism spectrum or have some sort of sensory differences than what we would consider typical if you're just in a regular clinic versus where I get, like these really interesting specialized cases. So not that you would change your clinical treatment pathway for someone with autism, but if they're really sensory sensitive most of them are wearing noise canceling headphones for our PT sessions and they're like reading my lips for me to tell them what I wanna do. Or we're in a treatment room so they're not in the busy gym space where there's weights and other kids and families and music playing. Sometimes we dim the lights, like there's a lot of sensitivity in general when they have this more complex pattern. And then on top of that is the dysautonomia and the POTS, which is something that I think I've been reading a lot more about and talking a lot more about and also talking with Dr Davenport about with the fatigue and just like the clusters that I was finding he's been like an incredible mentor to help with a lot of these patients that I'm very fortunate that we're in the same time zone.
Mark Kargela:
Yeah, no, there is always good that you have somebody you can text or message or something to bounce ideas off of. I know Todd, dr Davenport, students from great stuff as far as leading the way and doing a lot of things within some groups to help these folks that are dealing with some of these challenges to get better understood, better listened to and, hopefully, better helped overall.
Abby Gordon:
Specifically for him. I think we talk a lot about the differences between when you get a patient like I get my patients a lot of the time from the pain clinic and so our approach with a lot of kids with pain is to get them moving because they're fearful of movement because of the pain. But a lot of the time with the kids, like with either Stanlos or also with Long COVID there's a fatigue component that I think gets missed because they're not complaining about the fatigue, they complain about pain, it hurts, it hurts, it hurts. So I stay in bed and they're not really like focused on that fatigue. But then when we start getting them moving, the fatigue worries me a lot more because of the crashes that come when we start the exercise.
Mark Kargela:
Yeah, sometimes you find out the hard way that they're very exercise intolerant in the post-exercise malaise and I know there's another term I'm thinking of.
Abby Gordon:
Myalgic encephalomyelitis.
Mark Kargela:
Yes, exactly, chronic fatigue syndrome and those type of things. I get yeah, it is definitely had folks where you think you're starting at a low level and you think you're really bring, but they're just so reactive and that fatigue response is just extreme. So you can understand why people who deal with that are a little bit hesitant to engage in exercise and want to get after that. And that's where it really having a good ability to sit down and discuss with somebody, you know the approach, and starting very small and making sure they know and bringing those emotions out into the room. What's been your strategy? Like, do you feel like there's some things you found more helpful to like just sit down and level with somebody and really validate where they're at and validate their fear to engage with you? As a physical therapist, I found that to be helpful, just so they know. Hey, I get that you're afraid to engage and you don't want to have that fatigue response. You don't want your heart rate to spike to and have these syncopal episodes and all these different things. What's been your experience with just kind of that being a good human component of care?
Abby Gordon:
I mean, one big key experience is that a lot of these kids haven't had physical therapy ever before, so potentially I'm the first one they're meeting and sometimes when I say this it either sounds cocky or just a little bit extreme, like I don't think I'm the same as every other physical therapist. That's not to say better or worse. It's just that I'm willing to sit for a whole session and never make the patient move if that's the best thing for our therapeutic alliance and for their recovery. And that doesn't scare me when I think it probably would have. Eight years ago, at the beginning of my career, where it was like get your four units, bill, make sure you've touched them, make sure you know, you know ice has been on them, and then send them on their way when I work somewhere else. This is, my career has evolved and now you know I still bill for a session. But sometimes the session is us sitting and talking and coming up with a plan, and sometimes it's three or four and we try breathing strategies or education, but they don't know about vital signs. They don't know about they don't, they only are worried about the pain and they've been told that this is the problem. So I like don't want to just come at them with like you're wrong. They're children and their families are scared. So I have been trying to get the hashtag team therapeutic alliance to trend, but someday.
Mark Kargela:
Hey, we'll push it, we will. We will get that nudged forward, hopefully through the podcast a little bit, but I am fully on board. I love what you talk about. As far as spending an hour, I used to again, I'm blessed it sounds like you're blessed as well to work in this scenario where there's not this productivity pressure. I mean, obviously we can't just sit there and sip coffee and eat donuts with patients and, and you know, not do anything productive. But I think some of the most productive things are sitting down in front of somebody and validating what they're going through, listening to their story, putting everything that they're talking about on the table and making a plan up and, you know, starting with some basic breathing things and different things.
Abby Gordon:
Insurance has the biggest problem with this. They start denying it, saying you didn't do any movement and you don't have, you know, a measurement of strength. And I'm like kid can't get out of bed. What more do you need?
Mark Kargela:
Yeah, like, and that's where I've like because we've had, obviously, if students come through our clinic at Midwestern where I do, you know clinical mentoring and stuff and like sometimes functional, just like you do in the acute care hospital, like bed mobility and what kind of vital responses they have, and like you know you can talk about some of the basic things, like patient unable to sit upright without you know significant, you know distress or whatever it may be for that patient, where you can kind of bring it down to kind of just more basic mobility skills and then you know maybe some basic movement screening stuff. Just I've actually had some patients say you know we're going to make the insurance company happy. We're going to just have you do a few movements, safe movements that you can do. You're not here to push through anything today, so just let's see what you feel comfortable moving like and, you know, obviously make sure they're feeling like they're safe to do whatever we ask them to do. But yeah, it's. It is so frustrating the insurance company and because they I can understand the thought of what they're trying to do is try to have some quality control and make sure these, the money they're reimbursing us, is going to good care, but they just have this like algorithmic and it goes. I can obviously go into some tangents of how they take research and means statistics of group averages, which none of these folks are the average patient. They are, you know, dealing with some very challenging things that don't fit current. I mean, obviously we're going to do research and group research about on the groups of folks with this. But yeah, it is so frustrating when insurance companies are driving the. You know so much of the care which it should. It should be what's best for the patient, of course, but maybe too much for a utopian view, unfortunately. But I'm curious, kind of backing up a little bit, because you talked about some of the, the myriad of conditions that all of these folks, the GI contributions, this autonomia, all these different things I'm wondering, at Seattle Children's, or maybe you do it yourself, do you have like any specific educational things, maybe approaches you do, or maybe within your system to help people connect the dots to it? Because I've just found, and I'm curious, what your experiences, as well as like a lot of times they get to like the forest of trees of everyologist out there who's got the this is your GI tree and this is your, you know, cardiology tree and there's all these ologists who spoke is on one tree in a very complex forest. This is pretty much my shtick to the patients that I talk about. Like we're going to talk about all this stuff. All kind of relates of why the cardiologist needs to see, why the GI, why you're sensitive to smells and foods and you know all these different things. What's been your experience with that as far as people put things together for patients?
Abby Gordon:
Yeah, I mean the biggest thing for me is that I know how lucky I am that I'm in a hospital system, so like I'm in an outpatient clinic but I have directly across the hall orthopedics, cardiology. I have an eye doctor across the hall, like I'm in a space with a speech therapist, occupational therapist, a PT who does complete rehab, you know congenital PT. So I don't have to ever do those things and I only do sports and they don't ever want to see an ACL. So you know there's 75 specialties that come through my building in a week. That's not what everyone has, that's people don't. I can't even list them all, but I know that if a patient that I'm seeing has something strange, someone in the building is going to be able to help me figure out where they need to go, and I know that that is not what most people have. But I also think that it's a problem. I mean we've talked about a lot of the issues that our healthcare system has. It is a problem that I can see a patient who has something like post viral illness or Ehlers-Danlos, where I'm concerned about their heart rate and I send them to cardiology and cardiology gives them a halter monitor and it says normal rhythm of their heart rate, but at rest it ranges between 50 and 150 at rest. So the kid has no anatomical problems with their heart. And the doctor says go ahead with exercise. And I'm like but did you you saw the 150 at rest? Right? Like something doesn't feel right about this to me. And I hear you saying that their heart isn't damaged. But what about, like, how they feel in their brain when their heart is doing that? Because they don't get a subjective piece along with it. They get a mailed back halter monitor with a printout that says normal and they're like go ahead. And I think that's just the way our system is set up. It's not there. They're wonderful people, these doctors are so great. And when I respond back with I'm going to do exercise, but like, can we talk about this more? And does this really? Do you really see this all the time? Like there can't be. My heart rate doesn't go to 150 at rest.
Mark Kargela:
Yeah, I have to do some serious exercise to get that thing up to 150. Yeah, no, I agree, it's just that and it's a systemic thing. I agree with you. I mean no physicians out there to not listen to purpose. I'm not going to be listening to patients. I mean, I hope not. At least they're very good people have all the good intentions, but we have a system where it is so like objective check the box and just the ability for a physician to have time to like sit in front of somebody and really you know how's this been going for you when you're dealing with these cardiac issues. How does it make you feel? This must be very frustrating for you. I can't imagine how much stress this has put on you and your family. I know there's some unique docs who find a way, but it's a tough situation.
Abby Gordon:
It puts the pts, though, in a really interesting possible place. Like I benefit from this situation because we are not able to segmentalize that way with this patient population. Like you might be able to and I don't think we should, but you might be able to with somebody who, like, had ACL surgery. Like forget that they have three other extremities, a heart and a brain. But like, what about their cardio? Like we've seen a really good posts on social media from people who are focusing on specializing in ACL rehab, where it's like here's why you should go to somebody who only does this. And as somebody who rehabs post op ACLs, I like the acute phase where they're afraid to walk or not walking yet and I'm capable of doing late stage and doing dynamometry and testing and hop tests and jumping. But I get really concerned when I see them at four months out and nobody's done any cardio yet. Like why have we not got on your heart rate up or four months into this process? How much is that going to stink five more months down the road when you start to go back to sports? Like we as a profession have a lot of opportunity to get out of the silos that other specialties I think are stuck in because their jobs really need them to be like. I want the cardiologists to be an expert in cardiology, but I also want them to not forget the rest of the body happening. So it's really hard because I want it both ways and I want to practice both ways too. But I can't be a specialist in ACL rehab and all the musculoskeletal and also spend my time learning about these chronic pain conditions. There's no way it's. There's too many things to know.
Mark Kargela:
So yeah, it is an insurmountable mountain of research and things to learn, especially with chronic pain and worry. I mean conditions that we didn't even really consider in the clinic decade ago or so now are like commonplace, and how do we best treat these folks and how do we? And I agree, I think we're in a unique spot. I think that I love our unique position to the, where we can have that discussion about the forest and how you're seeing a bunch and how this regulation I mean I use a lot of stories about how your body in the haunted house versus the beach and sunset and how your autonomic system behaves differently. And then when you go through your journey, where do you think your body's? Hanging out at the haunted house and so just helping people key into like hey, this, you know, this frustrating, distressing, life altering, flip my life upside down thing is probably going to impact my ecosystem, my forest and then in turn, my GI, my, my cardiology, all these different things. So people can see that it's all kind of part of the picture. What are your thoughts on lifestyle medicine as far as? Where does that fit in your practice? Where do you see that with? You know kids can be challenging with with lifestyle. As far as you know, maybe some of the I know we've had kids where, you know, caffeinated drinks are in some of the monsters and all these things that don't really help matters when it's coming for for some of the stimulants. But what's been your experience and what maybe where does that fit for you?
Abby Gordon:
I actually really love this question. So I think that lifestyle medicine might have multiple definitions, but like every single new patient that I see for an evaluation, regardless of what they're coming in for, I'm going to ask them and remember I'm in pediatrics. So I don't say, do you eat fruits and vegetables, because yes or no answers don't get me enough information. I say what are your favorite fruits and vegetables? And if they can't come up with one of each, usually I worry that they're not having any. And there's no judgment here. They're just what are your favorites and because they also connect easily, these aren't scary questions. So it's really good for that therapeutic alliance to start with. So what are your favorite fruits or vegetables? What do you like to drink when you have a meal? And I'm looking for water because I want them to be hydrating, but I'm not going to judge when they do tell me that they drink Mountain Dew, as long as they're also drinking water. So I start with my hydration and nutrition and then we go to sleep and I say how do you sleep at night? What time do you go to bed? Are there other people in the room? A lot of them share rooms with siblings. It's just to get an idea of like, if we need to give attention to this part of your lifestyle, what things can we change and what can we not? But also I've had teenagers who tell me that they're sleeping, they're co-sleeping with a parent because the parent has cancer and it's like you're afraid you're going to lose your parent. Like how, I'm not, I'm going to tell you that it's better for your parent and for you, for everyone, to get better sleep, that maybe we do like bedtime story in your own bed. And then they leave Like we work on strategies because if they're not sleeping, everything is worse. So, yeah, I do hydration, nutrition, sleep. I ask everyone how's your mental health today, which I don't know why this is stigmatized How's your ankle sprain? How's your mental health today? Same question. And then I might ask something else about lifestyle, like what's your physical activity like? Unless they're an athlete who already told me all their sports, that's my lifestyle medicine. It only takes me about five minutes to do and a lot of the time it's interesting because the parent will be like huh, I didn't know, you like carrots. We don't really buy them that often, but I can buy you more, like I've had a lot of those and it kind of cracks me up.
Mark Kargela:
Yeah, I've definitely had similar where you're having discussions with kiddos and my mom and dad. Really it's interesting how sometimes parents are a little bit bamboozled by some of the answers and different things that their kids had Tough situation to be a parent and when you got your kid. I can't imagine if my daughter was dealing with some of the challenging things that some of our patients are dealing with.
Abby Gordon:
So it just really yeah, I mean as a non parent. I'm sure that I might come across interestingly to some parents because I think that I would do it in a certain way and maybe they don't. But it's hard to know what you would actually do when you're not raising a child. And I have a niece and nephew who I've watched grow up since they were born and who I would care about as if they were my own children, but I don't know that I would have raised them the same, even as my sister, just because we have different perspectives on everything. So for sure, I think lifestyle medicine matters potentially more than we give it credit for. But I even had a Twitter thread maybe a week ago, where a patient had come in. I saw her like a month and a half ago. She was having leg pain, like calf pain, bilateral, and she would have it every single night. And then the school year ends and she travels with her family. So I'd seen her before she traveled and I gave her a home exercise program and I wouldn't say she was very strong, but she was strong enough for, like her activities, I couldn't reproduce the symptom. She goes away with her family and she's gone for six weeks, has zero pain the entire time she's gone, comes back school starts, pain is right back where it was before and she tells me she doesn't eat at all before school or during school. She only eats after school. And I'm like I don't know if this is the problem, because pain is multifactorial, as we know. But I'm like I am going to say that we need to get some nutrition on board and like back to the pediatric because it was gone. So whatever made it gone isn't a PT thing. I can give you a thousand hill raises. I don't think your pain is going to go away.
Mark Kargela:
That's interesting you bring that up. I've had this discussion with colleagues as well about when folks go on vacation or do something where they escape the context of their four walls. I mean, obviously they escaped the context and got. Maybe they were eating well and sleeping well and doing all the things on vacation, and then school starts, like you said, and nutrition goes away and all these different things. I also just sometimes wonder how much were driven contextually of like I'm back to my life, where this is where all the things that weigh on me, all my distress lies, and all these four walls of all the challenges that I live were. You know, a vacation, disneyland, whatever it may be, is a break and I try to bring that into the room of like you know what's different on vacation.
Abby Gordon:
Yeah, they also said it was a lot hotter, just in general, like wherever they were was hot. And so when they come back a week later and they're like, look, I ate breakfast every single day for the last week because you told me I had to, my pain is still here and I'm like, what else is different when you're on vacation, because I'm happy to keep seeing you. You're a very nice kid. But, like, I don't think I'm going to solve this. This doesn't feel PT. But I feel like if you don't ask those questions and you observe that they don't hit the norms in the research of whatever number of heal raises you should have or whatever your hip extension strength should be, like you're just going to keep them in PT, doing exercises that potentially aren't going to touch whatever the problem is.
Mark Kargela:
Yeah, it's like you're not even asking to uncover what might be the root of it. If you because I think sometimes I know I did defaulted early in my career to what I felt comfortable with. I had my own exercise tree that I clung too tightly and that was the language I could speak with people, because it just. But obviously we know that there's this expansive force of a lot of things that go on with these folks, as you've already talked to you, a lot of the different systems that are impacted, a lot of the you know things. I like you know your questioning of mental health. I always joke with patients as, like ever, you get a physical. I think every you need to be getting the mental as well. I think I definitely am a firm believer and user of mental health as well, where I just think it's just helpful to have have that and addressing that is, and just see folks when you start unpacking some of those discussions of anxiety or depression and things.
Abby Gordon:
Yeah, you've had Rachel's office on here. You know you can't separate mental health from physical health. She's shouting it from the rooftops for a reason like we need to keep amplifying the message, because I think you asked earlier about, like the the aces, like the early trauma, early childhood trauma, and I don't feel like I see that necessarily a lot with the kids who are having long COVID or or or chronic fatigue. Necessarily I do certainly see kids who've had traumas, whether that's the reason they're in PT or it's just impacting them. But I have been surprised, as I've gone through my life and the experiences I've had, of how much mental health can really impact the way your body feels. You know, like I mean, I've talked about on Twitter plenty as well about grief and how grief comes out as pain in ways that like are that bring you to your knees, and I don't think we talk about some of these things nearly enough in PT education for the way that they come across in the clinic.
Mark Kargela:
Yeah, I just I see students and I definitely was one of these students as well when I was coming up through PT school when, like, emotions hit the room and when things beyond like what I was power pointed on, it was uncomfortable and I would just like abort mission and like let me just talk about what I know and kind of, I guess, invalidate it because I just didn't know how to address it. And now I think, like you said, like you got to have the ability to just have discussions and have conversations to where you just at least maybe open a door for to identify that, hey, maybe there's more to this than just you know how lax my shoulder joint is. Obviously that can be a part of it, not to say we just disregard that as well. But it's all of the things like Rachel talks about it. You can't separate the two. Yeah, sometimes as physios I think we just have this default sometimes. I know I did have just wanted to be a physical therapist when people aren't just physical, that their physical is so integrated with the mental and the psychological and all these different things. So I mean I'd love to talk a little bit about your thoughts on on pots, because I know you've been doing a lot of reading on it and it's one. Honestly I'm a little bit looking to pick your brain to help my practice out as well. I know you've probably read things that I haven't read in different things, but what's been your experience with you know kind of your approach and what you say? I know it's a variety and there's nobody know one patients the same. But what are maybe some common things you see in the clinic and maybe some common approaches you found can help some of these folks you know start moving in a better direction?
Abby Gordon:
Yeah, pots also way more frequent with the females than with the males and I think we're seeing potentially a spike around the time when they're hitting puberty. So I think that probably a lot of pts who aren't in the pelvic floor realm for get to ask questions about this. But I think we need to be asking about it if we're seeing patients who have this problem as well as stress, fracture type things. Like we need to be asking about energy availability because we know there's a cluster. Formerly the female athlete triad now read s like. I think that that's a consideration. So specific to pots, though definitely for girls teenage, not not young, young kids are they're all like the older teens, like I probably haven't seen even any that are really under like 15, so like they're been menstruating for maybe one or two years and then they start having it or they've had a viral illness, because it often comes with illness. The literature talks about different ways you can have POTS come on, which could be like deconditioning or immobilization following any sort of illness, or even surgeries, so like patients who've just been in bed for a long time. We had one patient who had that type of symptom presentation after they were hospitalized with cancer treatments where they were in bed doing chemo radiation and then they were discharged home and like really just couldn't get back to activity because of the dysautonomia. But that was deconditioning and they're so different in presentation and over time we were able to get them back to it. So it's interesting too, because some of the kids with POTS they get better and some of them just have to learn how to chronically manage it and I think that maybe is both things overlapping. So for sure I've posted several times question of whether or not it's in our scope of practice to like recommend hydration and electrolyte supplementation. Like I take electrolytes myself every single day because I stand at work for 10 hours and if I don't I am myself dizzy by the end of the day just because of gravity. And I made that change like five years ago and it was a game changer for my energy and my tolerance to the day. And so now it's like, hey, kids, are you drinking electrolytes? And when we do, and we have Gatorade in the clinic, so anyone who gets lightheaded and dizzy I'm like drink. And then when they feel better, it's kind of in the moment telling of oh, actually this has an impact. So for sure it's. We start with hydration, which usually they've been told by whoever diagnosed them with POTS. Sometimes we're doing compression wear, which are occupational therapists can do like fittings for compression garments. It kind of depends on how they're presenting. They don't, you don't always see like pooling in the legs or even color changes. But some kids with POTS have there's a name for it but I can't remember it like where their feet are blue and it's like it kind of looks almost like CRPS in that there's definite color change but it's like bilateral and it's in their feet, or it's kind of like a rain odds in the hands but like there's this change that's happening. So compression helps for some of them and those aren't PT things. And then we add in our PT things, like I like to do, resisted plantar flexion. However they can tolerate it. So if that's just active ankle pumps and they're not using resistance, that's fine. If it's a TheraBand, that's fine. If it's seated ankle pumps, that's fine. And if it's standing calf raises, it's fine. But everyone's getting one variation to just use that calf muscle pump. And then the level of exercise that we do depends on what they can tolerate. So if they can only really tolerate laying down exercises, we start with that and breathing strategies to try to calm the system down. But if they can tolerate seated, I wanna do the most that they're able to tolerate where they're not feeling terrible, cause they feel terrible if you really just push them through it.
Mark Kargela:
Yeah, yeah, we had spoke about it. It's the same kind of exercise progressions thought process. It's just you gotta bring it way back. Like you said, some of these folks could even try to sit upright to do exercise. That is just way, way too much for them and you have to really bring it down to mat-based exercises and, like you said, it could be as much as ankle pumps. Maybe get some bands involved. Yeah, the venous pooling things, it's interesting.
Abby Gordon:
Yeah, and I definitely try to reduce the amount of head up and down positioning so that could even be a squat or a sit to stand. Your head is moving up and down in space. It's interesting because these because they're kids sometimes they do things and you don't realize that this might be related. But like these kids lay on the floor, like if you tell them that they can take a break, they don't wanna sit on a treatment table or even in a chair, they wanna sit or lay on the floor and it's something about just like gravitational pressures and like feeling better. The number of kids who've laid on the floor in the clinic at first I was just like this is so weird. And then finally someone was like I just my head feels better down here than anywhere else and they wanna sleep on the floor at home. Like one of them told me they were crawling because if they got up they were just so miserable but crawling they could get around and do a lot more of their day. They would like lay on the floor to do their homework, to do school work. They would crawl to the table and like they'd sit up to eat because the family said you need to sit up to eat, but then they'd like crawl back to their bed and I was just like this is fascinating, and how do we help you so that you can stop crawling?
Mark Kargela:
Yeah, no, it is fascinating how you just start seeing these clinical patterns form of like. You see enough of a diagnosis, you start seeing these behaviors start to line up of like man. I haven't seen enough, probably to, but I definitely have had some folks were laying and not maybe on the floor we are.
Abby Gordon:
Our clinic maybe isn't as ideal for that, but I don't think mine's ideal for it, but when they do it I'm just like most kids don't do that.
Mark Kargela:
Yeah, it's not a common behavior, for sure, for sure. Yeah, no, it's a massively challenging situation that a lot of these kiddos and families are going through. What has been your experience with the family? Like, how have you you've found, like you know, there's the studies you know Adrian Lowe's been the one who kind of kicked him in front of me of like how mom and dad really are reacting to conditions really has a big effect, even like a year down the road of, like kids pain score. There's the parents psychosocial stress, anxiety scores like 24 to 40 hours after a thoracic procedure. I think it was in one study predicted this kids pain scores a year out from a procedure. So what has been your strategy with dealing with that dynamic?
Abby Gordon:
My strategy is to start with observing how they interact with each other, because usually the parents all come for the initial evaluation and our clinic policy is that if the kid is over 10, the parent doesn't have to be present for the session. But under 10, usually they don't have to be there, but they're invited to be there. And so when I feel like the parent is getting in the way, I'm not afraid to say hey, why don't you wait in the lobby so that we can tell you what we did afterwards? And that's my usual like get out. But I've also, because a lot of them are teens specifically with these conditions, I've asked the patient directly hey, are you ready to do this without your parent present yet? Because sometimes they're not ready to do it. They're fearful that they've had near-syncopal episodes or even true syncope. So I think they're fearful and early on. I'm not about to put them in situations where that's gonna happen, but you don't always know. And so if they don't trust me yet, they want their parent there. But once we build up the therapeutic alliance, usually they're like okay, what are you gonna do if this happens? And I'm like well, hopefully I catch you so you don't fall, and then I'll go get them. So we have to have those conversations, but I do think that half of the time, parents, in all of it, comes from a positive, loving, caring place of like does it hurt? Does it hurt? Does it hurt? Does that make you scared? Does that worry you? And I'm like you have to stop asking these questions. Like we need to get the focus a little bit away so that instead of them hearing what you're feeling, they can listen to their body. And I think once you explain it in that way, the parents are a little bit more ready to be like oh, they're 17. They should be able to like, at least feel. If they're a little fuzzy in their head with the because usually these syncopal episodes aren't they like stand up and they immediately fall back down. It's usually like I start doing something, I ramp up a little bit and then it's like oh, nope, can't do anymore. So they need to be able to pay attention to the signals, especially if they don't want to wear a watch that tells them their heart rate or if they're not so in tune to it at the beginning.
Mark Kargela:
Yeah, and when you're trying to teach breathing and relaxation strategies and things, and you got mom or dad, you know, in the room for good reasons, like you said, I mean it's all in love and it's all in care, but sometimes can spike the anxiety, you know, autonomic meter, by how they're reacting in the room and I think, having a play, you know, and it sounds like you have some great strategies, of course, with what you just said. But having the ability to kind of be able to be frank and have a discussion not in a mean way, but, you know, explain to parents how you know their reaction is going to ramp up the system or decrease the system Doesn't mean you don't care by any means, it just means we need to all modulate our response to it and let them start to get a little control of their body and not have external factors that are wanting to spike the accelerator again by, you know, somebody in their periphery you know doing, you know and again, and I and that's I always say you know this is all motivated good things. I mean you, obviously you care about your son or daughter. It's great, it's just we just need to make sure we're strategic in how we react and how we let the you know the kiddo kind of navigate some of this stuff and try to learn some ways, like you said, to get in tune with their body and not have some of these things that might deter.
Abby Gordon:
Yeah, my coworkers tell me this is when my East Coast is coming out, because it's not the same personality as some of them would have, where some of them just kind of are like it'll be fine and they just like kind of let it be on the side and I'm like, no, this is, this is getting in the way. But also sometimes we have to do the other way of like, hey, I need you to support your child in this way where they're trying so hard to let their kid be independent that the kid feels they don't have enough support. And I also think that that comes from a place of love of you wanting your 17 year old to be working towards being an adult, so you don't wanna be overbearing, but at the same time your kid is really struggling. So here are ways that we can, you know, put you into the mix so that they feel supported, without crossing all of the boundaries.
Mark Kargela:
Yeah, that would be something I'd have to be careful of my wife. It always gets annoyed with me, of like, whenever my daughter experiences anything, it's like she needs to navigate this, she needs to figure it out. We don't wanna get her freaked out about every scrape and bum she experiences in the world, because there are gonna be plenty to follow and so, yeah, no, I think it's great you brought that up as far as, like, sometimes you know you gotta figure out there's a balance. Sometimes it's too much, you know, distressing interaction and maybe sometimes not enough support where the person feels like they have that one little somebody to help shoulder some of the load of maybe what they're dealing with, which obviously can be very challenging. Abby, I wanna respect your time. I've really enjoyed the conversation immensely. I would love to hear I know you're gonna be doing some talks coming up. I'd love to hear what you're up to and what you got going on.
Abby Gordon:
Yeah, I'm excited to start getting invited to speak in a few places. This is new for me, so I'm looking forward to it. I'm gonna do a talk at UConn Physical Therapy, for they have a course that they wanted to do, a talk, sports physical therapy in the clinic versus on the sidelines, which I've given that talk once before to University of St Augustine, so we'll revamp that. And then also I'm gonna do a talk about POTS and Chronic Fatigue at Hartford Hospital while I'm home for Thanksgiving in Connecticut so little November busyness. And then, coming up in February, there's a conference in Minneapolis. That is the TRIA conference they're doing they haven't finalized, I think the theme is adolescent rehab this year. So they've asked me to speak and we haven't finalized the topic, but something about adolescent rehab versus adult rehab for potentially a certain condition. And then I'll have my first talk at CSM, which will be CRPS, and that's with Karen Litzie and Debra Sheldon. So I don't think you've had either one of them on your podcast, but they belong here.
Mark Kargela:
They do belong here. I know both Karen and Debra have met them both. They're great people and they definitely need to be on the list of folks that we're chatting with for sure. I'm looking. I won't be in CSM this year. I'm gonna be on a cruise because it's our 10th anniversary. So I got it, and it's in Boston. I mean, I love the Northeast, don't get me wrong. I'm not a hater on the East Coast, but I do like Southern East Coast a little bit more.
Abby Gordon:
Sure, who wants to go to Boston in February? This was not my choice, but it is home, connecticut's home, so I'll look forward to getting to see my family while I'm in the same trip.
Mark Kargela:
Well, awesome, I mean. Obviously you're doing great things and people are recognizing you're getting asked to talk and share your expertise. Where can folks? It sounds like X is the spot where you do a lot of your ponderings of things, and is that primarily where folks can kind of get in touch with you or see your content?
Abby Gordon:
Sure, yeah, I'm on there. I'm on Facebook, twitter, instagram, email. Find a way I'm responsive to everything. Linkedin People message me on LinkedIn a lot More than I would have guessed. I think it's probably because they search for, like, wnba stuff. So, yeah, wherever I'm communicative.
Mark Kargela:
Yes, you come across very well, you're well spoken and you can tell that your folks that are under your care are lucky to have you as their PT, and I really appreciate your time tonight and thanks for all the good stuff you're doing.
Abby Gordon:
Thanks for having me.
Mark Kargela:
All right. Well, we're gonna wrap it up with that. For those of you who aren't subscribed to the podcast, you need to get on your podcast vendor and subscribe to the podcast so we can get more folks like Abby's voice out there, so people with POTS and EDS and those folks and clinicians who are struggling with that can listen to it. If you're watching it on YouTube, we'd love to hear you or have you subscribe, or maybe just toss a comment in there. What's your experience with this? What have you found? Share some pearls. Maybe we can all learn. That's what this stuff is all about. So again, thank you for all your time. Thank you for spending some of your precious time and listening to the content we produce. We'll talk to you next week.
Speaker 2:
This has been another episode of the Modern Pain Podcast with Dr Mark Karjula. Join us next time as we continue our journey to help change the story around pain. For more information on the show, visit modernpaincarecom. Also visit the Pain Masterminds Network on Facebook for free education and resources. This podcast is for educational and informational purposes only. It is not a substitute for medical advice or treatment. Please consult a licensed professional for your specific medical needs. Changing the story around pain this is the Modern Pain Podcast.